Your doctor may suggest blood tests to check the levels of certain hormones and other thyroid cancer markers, if required (e.g. calcitonin and CEA or [Carcinoembryonic Antigen]).
Thyroid Cancer
Introduction
What is Thyroid Cancer?
It is a cancer the affects the thyroid organ in the neck. There are four main types of Thyroid Cancer: Papillary, Follicular, Anaplastic and Medullary. If this is not the cancer type you're looking for, please explore the information about other types of Head and Neck Cancers.
Cancer occurs when cells become abnormal, grow uncontrollably and have the potential to spread to other parts of the body. These cells build up to form a mass (or lump).
Papillary Thyroid Carcinoma / Cancer
This is the most common type of thyroid cancer (about 75% of all cases). It tends to grow very slowly, but often spread to lymph nodes. It can be cured or controlled in most people and is rarely fatal
Follicular Thyroid Carcinoma / Cancer
This accounts for about 5-10% cases. It grows slowly and tends to stay in the thyroid, however it can spread to the lungs or bones if diagnosed late. If diagnosed early, most people with follicular Thyroid Cancer can be treated successfully.
Anaplastic Thyroid Carcinoma / Cancer
This type of thyroid cancer is rare (less than 1%) but is very aggressive and can be challenging to treat.
Medullary Thyroid Carcinoma / Cancer
This is different to other thyroid cancers because they develop in cells called ‘C cells’ that do not produce thyroid hormone and can be due to having an underlying genetic predisposition. All patients who develop this type of thyroid cancer should be assessed to decide if they need genetic testing.
There is also Poorly Differentiated Thyroid Cancer, which makes up to 5% of Thyroid Cancer and usually occurs in older people. It can frequently be non iodine-avid.
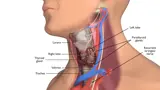
What is the thyroid?
The thyroid gland lies at the base of the neck. It is shaped like a butterfly and wraps around the windpipe (trachea) beneath the voice box (larynx).
The parts of the thyroid are:
- wings of the butterfly (left and right lobes)
- body of the butterfly (isthmus, joining the left and right lobes)
- there is a small part that lies over the voice-box (pyramidal lobe)
When the thyroid is larger than normal it is called a goitre. Lumps in the thyroid are called nodules. Most thyroid nodules are benign but some can be cancerous.
Here is a 3D video explainer that explains the thyroid and Thyroid Cancer further:
What does the thyroid do?
Glands that release hormones into the blood stream are called endocrine glands, the thyroid is the largest endocrine gland of the body.
There are two types of thyroid hormone, tri-iodothyronine (T3) and thyroxine (T4).
These hormones control the speed at which the cells work (metabolism), and are important in brain development and growth in children. These hormones also determine how sensitive other organs are to endocrine hormones. Thyroid hormone is made in cells called follicular cells.
The amount of thyroid hormone in the blood stream is controlled by the pituitary gland. The pituitary gland, is a small endocrine gland that sits under the brain. It releases a hormone into the blood called thyroid stimulating hormone (TSH). When doctors order thyroid tests, they will look at all three of these hormones (T3, T4 and TSH) but TSH is the most important.
- Too much thyroid hormone is called hyperthyroidism or an overactive thyroid. This can lead to heart palpitations, trouble sleeping, shaky hands, muscle weakness, nervousness or anxiety, feeling hot and problems with your menstrual periods.
- Not enough thyroid hormone is called hypothyroidism or an underactive thyroid. This can lead to weight gain, lethargy, intolerance to cold weather, depression, constipation and problems with hair loss and dry thyroid.
Diagram of the thyroid and surrounding areas:
What causes Thyroid Cancer?
Doctors often can’t explain why a person gets cancer. But we do know what makes some cancers more likely.
The two main causes of Thyroid Cancer are:
- Being female — In Australia women are about four times more likely than men to get Thyroid Cancer
- Age — while Thyroid Cancer can occur at any age, it is most common in people aged 40–60 years.
Having a diet low in iodine also increases risk of Thyroid Cancer, but this is rare in Australia as iodine is added to salt and other foods.
Other factors that increase the risk of Thyroid Cancer include:
- Radiation — this is a very important risk factor for Thyroid Cancer, either because of medical treatment (particularly low dose radiation treatment in childhood), or from environmental exposure such as atomic explosions or nuclear fallout.
- Having a non-cancerous (benign) thyroid disease — like an enlarged thyroid (goitre), thyroid nodules (adenomas) or inflammation of the thyroid (thyroiditis), or having one of these conditions in your family.
- A family history of Thyroid Cancer or an inherited gene change (mutation) in the RET oncogene (a protein coding gene).
Symptoms and Symptoms of Thyroid Cancer
The signs and symptoms of thyroid cancer depend on where the cancer is, its size and how far it has spread in the body.
The most common sign is a lump or swelling in the middle of the neck (where the thyroid is). Some Thyroid Cancers can spread to the lymph glands and cause a lump in the side of the neck.
Lumps in the thyroid are called nodules, but most nodules are not cancerous.
Other less common symptoms of Thyroid Cancer are:
- change in voice due to damage of the voice box nerve which runs behind the thyroid gland
- difficulty swallowing due to compression of the swallowing tube (oesophagus)
- difficulty breathing, or shortness of breath due to involvement of the windpipe which sits underneath the thyroid gland
- pressure in the neck when lying down
Most Thyroid Cancers do not produce any symptoms and are commonly found incidentally on scans (ultrasound or CT scan) for other conditions.
Most often these symptoms are not from Thyroid Cancer. However, if you have any of these symptoms for more than a few weeks, talk to your doctor as early as possible. They may be able to help diagnose and treat you.
Tests for Thyroid Cancer
It is important that your doctor establishes the diagnosis of Thyroid Cancer, assess the size of the cancer and whether it has spread to the lymph nodes in the neck or elsewhere in the body.
To answer these questions your doctor will need to do the following things:
- talk with you about your medical history. This includes signs you may have noticed, any health conditions, medications you are taking, and whether you smoke or drink alcohol
- perform a physical examination by feeling and looking at your neck and throat
- order diagnostic tests, which may include scans
Thyroid Cancer is often found when someone has a scan of the neck area. However, there are lots of different tests that can be used to confirm a diagnosis of thyroid cancer. Not everyone will need to have every test for thyroid cancer. Your doctor will recommend tests that are right for you.
Common tests include:
Your doctor may suggest ultrasound to produce pictures of the thyroid and nearby lymph nodes, to look at any nodules (lumps) in the thyroid and also in the lymph nodes.
Your doctor will use a very thin flexible tube with a tiny light and camera on it, and pass it through your nose to see down the back of your throat to check the function of vocal cords as nerves to your voice box may be affected by thyroid cancer.
This involves removing a small piece (sample) from the cancer. The sample is then examined under a microscope to check for cancer cells. This is often the only sure way to tell if you have cancer.
Your doctor may recommend:
Your doctor may recommend a Fine Needle Aspiration or FNA. This is used when there is a lump (enlarged lymph node) in your neck that could have cancer cells in it. During the procedure, your doctor will take some cells (a very small sample) from the lump using a needle. This is done by a radiologist, clinician or pathologist using an ultrasound to see that the needle is in the right spot. You may feel a bit uncomfortable during the biopsy.
Your doctor may suggest thyroid scan if blood tests indicate an overactive thyroid. This involves injecting a small amount of radioactive liquid (such as iodine) into your arm prior to a gamma camera scan.
This uses X-rays to take pictures of the inside of the body. If the person has cancer, a CT scan can help the doctor see where it is, measure how big it is, and determine whether it has spread into nearby organs or other parts of your body.
MRI (Magnetic Resonance Imaging) Scan
This uses magnetic fields to take pictures of the inside of the body. This helps the doctor see how far a cancer has grown into the tissue around it.
PET (Positron Emission Tomography) Scan
This is a whole body scan that uses a radioactive form of sugar which can show if thyroid cancer has spread elsewhere in the body.
Treatment Options for Thyroid Cancer
Following a diagnosis of Thyroid Cancer, your cancer care team will discuss the treatment options including the possibility of participating in a clinical trial that is suitable for you. This is also a good time to consider if you would like a second opinion.
The most suitable treatment for Thyroid Cancer depends on many things including:
- size and location of the cancer
- whether the cancer has spread
- personal factors (e.g. age, general health and treatment history)
- treatments available
- your preferences for treatment
Surgery is the main treatment for people with thyroid cancer. The aim of treatment is to surgically remove all thyroid cancer cells. Many people with thyroid cancer also receive radioactive iodine and thyroid hormone replacement. Some people will need other treatments such as radiation. Adding another form of treatment is known as adjuvant therapy.
Radioactive iodine treatment is a form of internal radiation therapy, typically taken in a gel tablet form (with 1 to 3 days in hospital), to destroy any residual thyroid tissue and thyroid cancer cells left behind after surgery.
Thyroid hormone replacement therapy is needed in patients who have had all of their thyroid removed. This is to replace the thyroid hormone in the body and to help slow the growth of any cancer cells to reduce the risk of the cancer coming back.
The treatments listed apply to most thyroid cancers.
How can I Prepare for the Surgery?
Your doctor will explain details of the surgery, general risks and side effects of surgery. Ask your doctor if you have questions. They may recommend:
- stopping blood thinners (e.g. aspirin) before surgery to reduce the risk of bleeding
- special stockings to reduce the risk of blood clots
- early mobilisation (i.e. not staying in bed) to reduce the risk of blood clots and chest infection
- antibiotics to lower the risk of wound infection.
If you smoke, it is important that you consider stopping smoking before starting treatment to help reduce the risk of infection and recover after your treatment.
Surgery for Thyroid Cancer
The main treatment for Thyroid Cancer is surgery. There are a number of operations that can be used to remove Thyroid Cancer . The type of operation used will depend on the size and location of the cancer.
The different surgical options for Thyroid Cancer are:
This is the removal of the thyroid gland from the neck. If the entire thyroid gland is removed, it is called a total thyroidectomy. If only some of the thyroid gland is removed, it is called a partial or hemi-thyroidectomy.
Download PDF - Neck Dissection
Download PDF - Return to Activity Following Neck Dissection
This involves removal of lymph nodes from the neck. This is important even when there is no sign of cancer in the lymph nodes on your scan, because there is a risk of microscopic cancer in the lymph glands of the neck.
Side Effects of Surgery
Treatment for thyroid cancer may lead to a number of side effects . You may not experience all of the side effects. Speak with your doctor if you have any questions or concerns about treatment side effects.
Guide to Thyroid Hormone Replacement Therapy
Thyroid hormone replacement helps to keep your body’s metabolism at a normal healthy rate. If you do not have enough thyroid hormone (hypothyroidism) you may have symptoms such as weight gain, constipation, brittle and dry hair, sluggishness and fatigue. Heart problems can occur in severe cases. Too much thyroid hormone (hyperthyroidism) may cause symptoms such as weight loss, chest pain, rapid or irregular heartbeat and feeling hot.
For thyroid hormone replacement, your doctor will prescribe a tablet (every day for the rest of your life). You should take the tablet at the same time every day. Speak to your doctor about all other medications that you take, including dietary supplements such as iron and calcium.
- Your doctor will suggest blood tests to monitor your thyroid hormone levels, to help them adjust the dose. Don’t stop taking the thyroxine medication without discussing it first with the doctor.
- Tell your doctor if you are pregnant as a higher dose may be needed.
- The dose of thyroid hormone needed is different for every person and may change as a person ages. Talk to your doctor about any signs to look out for.
Taking thyroxine also helps to reduce the risk of cancer coming back, or recurring, by lowering the thyroid stimulating hormone made by your body which can stimulate thyroid tissue growth. Lowering the thyroid stimulating hormone (TSH) by taking thyroxine is called ‘TSH suppression’. A higher dose of thyroxine will be used for TSH suppression, if there is a higher risk of the cancer coming back (recurring). Your doctor will monitor the level of your TSH. Sometimes the dose will need to be adjusted, but it is important you do not increase your dose of thyroxine without speaking to your specialist.
Radioactive Iodine Treatment
Radioactive iodine can be used as a radiation treatment for Thyroid Cancer since the thyroid gland in particular takes up iodine in the body.
The cancer cells take up radioactive iodine (called iodine–131) which causes the cancer cells to die. It is usually given to destroy remaining thyroid cells, not removed by surgery and any that may have spread.
Radioactive iodine treatment is an option only for some people with the papillary and follicular types of thyroid cancer and often starts at least 4-5 weeks after surgery.
For women who are pregnant and those who are breastfeeding, radioactive iodine treatment is not suitable. Your doctor will recommend stopping radioactive iodine treatment, before starting treatment.
Guide to Radioactive Iodine Treatment
How to prepare for radioactive iodine treatment
- For about 2 weeks before treatment, you will need to avoid foods high in iodine such as seafood, iodised salt, some dairy food and any food coloured pink with the additive E127. You need to have a low iodine diet because too much iodine in your body can stop the treatment working well. Your cancer care team will provide you with advice on foods to avoid.
- You will need to either stop taking thyroid hormone replacement pills temporarily, or have injections of thyroid stimulating hormone (Thyrogen) while taking the hormone replacement. This is to increase the thyroid stimulating hormone in your body, and your cancer care team will discuss the best option available for you.
- If you have the option of stopping thyroid hormone replacement during the preparation, there may be some side effects due to hypothyroidism such as tiredness.
After radioactive iodine treatment
- After the radioactive iodine treatment, you will have a full body radio-isotope scan, using a small amount of radioactive liquid. The scan can help detect if any cancer cells are left or if the cancer has spread. The scan is painless and causes few side effects, and you will not be radioactive after the scan.
- At home you may need to continue safety measures such as sleeping alone, washing your clothes separately and preparing your own food. You may be advised to sit to pass urine, shut the lid and flush the toilet several times.
- You may be advised to take precautions to avoid pregnancy for a while after treatment, If you or your partner want to have a baby after radioactive iodine treatment, you should talk to your doctor for advice about suitable timing.
Radiation Therapy for Thyroid Cancer
Radiation therapy is rarely used as the main treatment in thyroid cancer. Sometimes external beam radiation therapy (X-rays applied from outside the body) may be used after surgery (adjuvant radiation therapy). Radiation therapy can be used in the following ways:
Adjuvant
This is when radiation therapy is given after the surgical removal of thyroid cancer to kill cancer cells that may not have been taken out during surgery. When used, it usually starts about 4 weeks after surgery to allow recovery from surgery. Radiation therapy treatment usually lasts for about 6 weeks.
Palliative
In cases where a cure is not possible, radiation therapy is used to relieve symptoms of advanced thyroid cancer. Symptoms that may require palliative radiation therapy include pain, bleeding, airway obstruction and swelling.
Side Effects of Radiation Therapy
The side effects of radiation therapy start around two weeks into treatment and progress through treatment to peak in the last week just after treatment ends. The side effects start to improve 2–3 weeks after the end of treatment.
Side effects associated with radiation therapy depend on:
- the dose of radiation therapy
- the area being treated
- whether or not chemotherapy is added to the radiation therapy.
Systemic Treatment - treatment that helps the whole body
Systemic treatments are usually only required when thyroid cancer spreads or is very aggressive. Systemic therapies used for the treatment of thyroid cancer most commonly refer to targeted therapy, and uncommonly chemotherapy.
Targeted Therapy
When Thyroid Cancer spreads or if it becomes resistant to radioactive iodine, there are a number of targeted therapies available in the form of a tablet, that “target” and stop key growth pathways that thyroid cancers use to grow and spread. For example, these targets often refer to known genetic mutations (abnormalities) that occur in Thyroid Cancer that are responsible for driving cancer growth and spread. Targeted therapy, often called “tyrosine kinase inhibitors” or “TKIs” for short, can be effective to control cancer growth for some time. However, like all tablets side effects can occur so the timing of starting the tablet will be an important decision that your doctor will discuss with you. Your doctor may need to organize the genetic testing of your cancer .
Chemotherapy
Chemotherapy works by destroying or damaging cancer cells. Chemotherapy is not commonly used for the treatment of most thyroid cancers. However, occasionally it is considered for people with advanced thyroid cancer who are no longer responding to other treatments or if you have anaplastic thyroid cancer.
Clinical Trials and Other Treatment Including Immunotherapy
Fortunately, advances in the treatment of cancer are part of routine cancer care. You may be offered participation in a clinical trial if available and relevant for your cancer type, which aim to discover or establish new treatment options for people with your type of cancer. The advantages and disadvantages of trial participation will be discussed with you before you are able to consider participation. Clinical trials are vital to help establish the best treatment for different types of cancer and can be a means of accessing new therapies that have proven value. If a treatment hasn’t been tested in enough patients to know it is safe or effective, then these treatments need to be tested in a clinical trial to prove whether they are truly beneficial for the treatment of your cancer.
Questions to Ask
- Exactly what type of Thyroid Cancer do I have? Where is it located?
- Why did I get this cancer?
- What stage is the cancer?
- What are my treatment options? Which treatment do you recommend for me and why?
- Have you discussed my case at a Multidisciplinary Team meeting and what were the recommendations?
- Who will be part of the cancer care team, and what does each person do? Should I see another specialist before treatment, such as a radiation oncologist, medical oncologist, plastic surgeon, dentist, dietitian or speech pathologist?
- What are the possible side effects of treatment in the short- and long-term? How can they be prevented or managed?
- Will the treatment affect my ability to eat, swallow, or speak? Will I need a feeding tube?
- What will happen if I don't have any treatment?
- How much will the treatment and/or operation cost? Will Medicare or my health insurance cover it?
- What follow-up tests will I need? How often will they be?
- Am I suitable for any clinical trials?
- What lifestyle changes (diet, exercise) do you recommend I make?
- Who can I call if I have any problems or questions?
- Where can I find emotional support for me and my family? Is there a support group or psychologist you can recommend?
- If I wanted to get a second opinion, can you provide all my medical details? Do you mind if I get a second opinion?
Follow-Up Care
You will have regular check-up after your treatment for Thyroid Cancer. It is important to keep up with follow-up meetings, to make sure that if the cancer comes back, it is caught and treated as early as possible. If you have any concerns between visits, you should contact your doctor.
At your follow-up visit, your doctor will perform a physical examination (e.g. feel your neck). Depending on the type of thyroid cancer, and the risk of cancer returning, your doctor will recommend scans and blood tests.
You May Have the following Tests and Scans:
Blood Tests
Thyroid hormones and TSH are measured as needed, to check you are on the right dose of thyroid hormone replacement and to monitor thyroid stimulating hormone (TSH). The dose of thyroid hormone may be adjusted for your needs, including changes with age.
TSH is monitored for TSH suppression or lowering. TSH suppression aims to reduce the risk of cancer coming back, and is used particularly for patients with a higher risk of recurrence.
Thyroglobulin. If you have been treated for papillary or follicular cancer, blood tests will be done for thyroglobulin, which is a tumour marker protein made by thyroid cells. Levels are very low if the thyroid gland has been removed and may rise if the cancer comes back. Anti-thyroglobulin antibodies may also be measured.
Sometimes the doctor may decide to measure stimulated thyroglobulin, as the test can be more accurate. The doctor would give you instructions about any changes in your medication needed before this test.
Calcitonin and a tumour marker protein called carcinoembryonic antigen (CEA) will be measured for patients treated for medullary thyroid cancer. Levels may rise if the cancer comes back.
Neck Ultrasound
An ultrasound of the neck is used to check the area where the thyroid was removed to see if there is any cancer growing in the thyroid bed. It is also used to check your lymph glands around the neck.
Radioistope Scan
A radioisotope scan is used to check of there are any cancer cells in your body. A small amount of radioactive liquid (eg iodine-131) is injected into a vein and after about 20 minutes you will lie under a gamma camera machine.
You may need to change your medications before a radioisotope scan to help the cancer cells take up the radioactive iodine and make the test more accurate. Your doctor would give you instructions on any changes needed.
The scan measures how much radioactivity has been taken up by the thyroid and also helps to see if the cancer has spread.
The scan is painless and has few side effects. You will not be radioactive after the scan.
CT, PET or other Scans
You may have a CT or PET scan if cancer cells are found elsewhere in your body or if further testing is needed.
CT or MRI scans are not used routinely. They may be used when the blood tumour markers suggest the cancer has come back, but it has not shown up on the ultrasound or radioisotope scan. These scans may also assist in planning any further surgery.
Diet and Nutrition
It is important for people with thyroid cancer to stay well-nourished and to avoid unplanned weight loss. If you can’t eat or drink enough, you may become malnourished or begin to lose weight. In this case, your healthcare team may consider feeding you through a tube for a period.
Maintaining good nutrition is important to help:
- ensure you get through treatment
- reduce your risk of infection
- recover more quickly
- keep your strength and energy levels up
What can I do to help my diet and nutrition?
To help your body recover from surgery, you need to be well nourished. You can keep well-nourished and hydrated during and after your treatment by:
- eating a diet high in protein and calories (energy)
- eating small meals or snacks, more frequently
- drinking nourishing fluids, such as milk, milkshakes, smoothies or juice . Your dietitian may also recommend nutritional supplement drinks which are high in protein and energy.
You may need to make changes to the types of food you eat. If you have a sore throat, you may want to avoid foods that irritate, such as citrus or vinegar, and hard foods, such as chips or toast. Try to swallow gently and to eat small amounts of healthy, nutritious food.
For patients preparing to have radioactive iodine treatment
For about 2 weeks before treatment, you will need to avoid foods high in iodine such as seafood, iodised salt, some dairy food and any food coloured pink with the additive E127. You need to have a low iodine diet because too much iodine in your body can stop the treatment working so well. Your health care team will provide you with advice on the foods to avoid.
Visit the Cancer Council website for further information about diet and nutrition.
On this page