Throat Cancer
Introduction
What do we mean by 'Throat Cancer'?
Throat Cancer is a colloquial umbrella term that encompasses several specific types of cancer in the neck. These include Hypopharyngeal Cancer, Nasopharyngeal Cancer, Oropharyngeal Cancer and Laryngeal Cancer.
To read in more detail about any of these cancer types, click on the relevant links throughout this article. If none of these are the cancer type you're looking for, please explore the information about other types of Head and Neck Cancers.
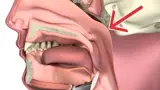
The medical term for the throat is the pharynx. The pharynx has three parts:
- nasopharynx (upper throat, behind the nose)
- oropharynx (mid throat, including base of tongue and tonsils)
- hypopharynx (lower throat)
The hypopharynx, the lowest part of the throat, leads into the oesophagus, which is sometimes also called the gullet and is located behind the larynx (voice box).
What causes Throat Cancer?
Cancer occurs when cells become abnormal, grow uncontrollably and have the potential to spread to other parts of the body. These cells build up to form a mass (or lump).
Doctors often can't explain why a person gets cancer. But we do know what makes some cancers more likely.
The possible causes of Throat Cancer vary depending on the exact type of cancer it is.
Let's take a look at the precise types of Head and Neck Cancer in the throat.
Types of Throat Cancer
Nasopharyngeal Cancer
Nasopharyngeal Cancer is a type of throat cancer that forms in the nasopharynx, which is highest part of the throat — in or behind the nose.
Causes of Nasopharyngeal Cancer
The main causes of Nasopharyngeal Cancer are viruses, in particular the Epstein-Barr virus (EBV), and smoking. Other factors that increase the risk of Nasopharyngeal Cancer are:
- Age
- Eating a lot of salt, cured fish and meat
- Being male
- Being from Southern China or South East Asia
Here is a 3D video explainer about Nasopharyngeal Cancer:
Oropharyngeal Cancer (including Tonsil Cancer)
Cancer that starts anywhere in the oropharynx is called Oropharyngeal Cancer. Your doctor may also call it by the part it has grown in, like tonsil or tongue base cancer.
The oropharynx is the middle part of the throat, that is directly behind the mouth. It is made up of four parts:
- sides of the throat, including the tonsils
- base of the tongue (back third of the tongue), sitting above the voice box
- soft roof of the mouth (or the soft palate) and the fleshy part of skin hanging from the roof (or the uvula)
- back wall of the throat (or the posterior pharyngeal wall)
Causes of Oropharyngeal Cancer
The main causes of Oropharyngeal Cancer are
- human papillomavirus (HPV)
- smoking
- drinking alcohol
Here is a 3D video explainer about Oropharyngeal Cancer:
Hypopharyngeal Cancer
Hypopharyngeal Cancer refers to cancer that forms in the hypopharynx (lower part of the throat). The hypopharynx is a horseshoe shaped that sits behind and around the larynx (voice box). It's job is to direct food into the oesophagus (or food pipe).
Hypopharyngeal Cancer often occurs in pockets on either side of the hypopharynx (called the piriform sinuses).
Causes of Hypopharyngeal Cancer
The two main causes of Hypopharyngeal Cancer are smoking and drinking alcohol. Get information about quitting smoking and reducing how much alcohol you drink.
Other factors that may increase the risk of Hypopharyngeal Cancer are:
- Being male
- Age
- Exposure to certain substances
- Poor diet
Here is a 3D video explainer about Hypopharyngeal Cancer:
The larynx (or voice box) is an organ in the front of the neck. It is made up of cartilage (a firm tissue), muscles and ligaments which move to make different sounds and protect your lungs when swallowing. The cartilage in front of the larynx is sometimes called the Adam’s apple.
There are many types of tumours (lumps) that occur in the larynx. Many of these are not cancers but are what doctors call ‘growths’ or ‘lesions’. Common examples include vocal cord nodules or papillomas.
Causes of Laryngeal Cancer
The two main causes of Laryngeal Cancer are smoking and drinking alcohol. Get information about quitting smoking and reducing how much alcohol you drink.
Other factors that may increase the risk of laryngeal cancer are:
- Being male
- Age
- Family history
- Low immunity
- Exposure to asbestos
Here is a 3D video explainer about Laryngeal Cancer:
Signs and Symptoms of Throat Cancer
The signs and symptoms of any type of cancer in the throat, will depend on where the cancer is, its size and how far it has spread in the body.
'Throat Cancer' is a colloquial umbrella term that is not usually used by medical practitioners. To more accurately describe the symptoms and signs of a cancer in the throat, it's best to refer to the specific cancer type. For example, Hypopharyngeal, Nasopharyngeal, Oropharyngeal and Laryngeal Cancers.
Below, you will find the signs, symptoms and tests of these main head and neck cancers that are sometimes referred to generally as 'Throat Cancer'. These summaries are brief introductions. You are encouraged to read more detailed information at the links in each section.
Most often the signs below will not be symptoms of cancer. However, if you have any of these symptoms for more than a few weeks, talk to your doctor as early as possible. They may be able to help diagnose and treat you.
Nasopharyngeal Cancer
Nasopharyngeal Cancer is a type of throat cancer that forms in the nasopharynx, which is highest part of the throat — in or behind the nose.
Symptoms and Signs of Nasopharyngeal Cancer
The signs and symptoms of Nasopharyngeal Cancer depend on where the cancer is, its size and how far it has spread in the body.
Common signs and symptoms include:
- nasal obstruction or stuffiness
- frequent nose bleeds
- blocked ear, decreased hearing or ringing in the ear (especially on one side only)
- a lump in the neck
- frequent headaches
- numbness in the face
- blurred or double vision
Tests for Nasopharyngeal Cancer
The most common tests for Nasopharyngeal Cancer are:
- Nasoendoscopy
- Biopsy
- CT (Computed Tomography) Scan
- MRI (Magnetic Resonance Imaging) Scan
- PET (Positron Emission Tomography) Scan
Oropharyngeal Cancer (including Tonsil Cancer)
Oropharyngeal Cancer includes is cancer that starts anywhere in the oropharynx. Your doctor may also call it by the part it has grown in, like tonsil or tongue base cancer.
Symptoms and Signs of Oropharyngeal Cancer
Oropharyngeal Cancer can show up in different ways. Common signs and symptoms may include:
- a sore throat that doesn’t go away
- a sore (like an ulcer) in the throat
- a lump in the throat
- a lump in the neck (this is common and may be the only sign in many people)
- trouble swallowing food, or moving the tongue
- trouble opening the mouth
- trouble breathing
- noisy breathing
- ear pain
- coughing up blood
- voice change
- unexplained weight loss
Tests for Oropharyngeal Cancer
The most common tests for Oropharyngeal Cancer are the same as those for Nasopharyngeal Cancer:
- Nasoendoscopy
- Biopsy
- CT (Computed Tomography) Scan
- MRI (Magnetic Resonance Imaging) Scan
- PET (Positron Emission Tomography) Scan
Hypopharyngeal Cancer
Hypopharyngeal Cancer refers to cancer that forms in the hypopharynx (lower part of the throat).
Symptoms and Signs of Hypopharyngeal Cancer
Some people with Hypopharyngeal Cancer might not experience any symptoms at all. However, common signs and symptoms include:
- hoarseness of voice
- pain on swallowing
- difficulty swallowing
- sore throat or pain in the ears (particularly on one side)
- a lump in the neck (swollen lymph nodes or glands)
- noisy or difficult breathing
Tests for Hypopharyngeal Cancer
It's important that your doctor establishes the diagnosis of Hypopharyngeal Cancer, assesses the size of the cancer and whether it has spread to the lymph nodes in the neck or elsewhere in the body.
Not everyone will need to have every test for Hypopharyngeal Cancer. Your doctor will recommend tests that are right for you. The most common tests for Hypopharyngeal Cancer are:
- Biopsy
- Blood Tests
- CT (Computed Tomography) Scan
- Nasoendoscopy
- MRI (Magnetic Resonance Imaging) Scan
- PET (Positron Emission Tomography) Scan
- Ultrasound Scan
Laryngeal Cancer
The larynx (or voice box) is an organ in the front of the neck. There are many types of tumours (lumps) that occur in the larynx. Many of these are not cancers but are what doctors call ‘growths’ or ‘lesions’.
Symptoms and Signs of Laryngeal Cancer
The most common early symptom associated with Laryngeal Cancer is hoarseness or change in voice.
Other signs and symptoms include:
- pain on swallowing
- difficulty swallowing
- sore throat or pain in the ears
- a lump in the neck (swollen lymph nodes or glands)
- noisy or difficult breathing
Tests for Laryngeal Cancer
The most common tests for Laryngeal Cancer are the same as those for Nasopharyngeal and Oropharyngeal Cancers:
- Nasoendoscopy
- Biopsy
- CT (Computed Tomography) Scan
- MRI (Magnetic Resonance Imaging) Scan
- PET (Positron Emission Tomography) Scan
We encourage you to read the more detailed information on each cancer type.
Questions to Ask
- Exactly what type of cancer do I have? Where is it located?
- Why did I get this cancer? Is it related to the HPV virus?
- What stage is the cancer?
- What are my treatment options? Which treatment do you recommend for me and why?
- Have you discussed my case at a Multidisciplinary Team meeting and what were the recommendations?
- Who will be part of the cancer care team, and what does each person do? Should I see another specialist before treatment, such as a radiation oncologist, medical oncologist, plastic surgeon, dentist, dietician or speech pathologist?
- What are the possible side effects of treatment in the short- and long-term? How can they be prevented or managed?
- Will the treatment affect my ability to eat, swallow, or speak? Will I need a feeding tube?
- What will happen if I don't have any treatment?
- How much will the treatment and/or operation cost? Will Medicare or my health insurance cover it?
- What follow-up tests will I need? How often will they be?
- Am I suitable for any clinical trials?
- What lifestyle changes (diet, exercise) do you recommend I make?
- Who can I call if I have any problems or questions?
- Where can I find emotional support for me and my family? Is there a support group or psychologist you can recommend?
- If I wanted to get a second opinion, can you provide all my medical details? Do you mind if I get a second opinion?
Follow-Up Care
You will need regular check-up of your throat and neck after for Throat Cancer. This will include a physical exam and checking your nose and throat using a thin, flexible tube with a light and camera (nasendoscopy). You may need to have follow-up CT, MRI or PET scans to catch any early signs of reappearance of the cancer. It is important to keep up with follow-up appointments to make sure that if the cancer comes back it is caught early and can be treated. If you have any concerns between appointments you should contact your doctor.
People who smoke and/or drink alcohol can reduce the risk of their cancer coming back or getting a new cancer if they quit smoking and reduce the amount of alcohol they drink. Ask your cancer care team for advice if this applies to you.
Importance of Ongoing Dental Care
A dentist plays an important role in your Head and Neck Cancer treatment. Side-effects can often be prevented or reduced through regular dental check-ups before, during and after cancer treatment. After your treatment, you should visit the dentist every six months for a check-up because the side effects of radiation therapy on your teeth can last for your whole life.
Mental Health for People with Cancer
Sometimes this is referred to as psychosocial aspects or survivorship.
Being diagnosed with cancer and having treatment can lead to extra worries or concerns for you and the people caring for you. Depending on the treatment, you may experience any of the following:
- low mood or depression
- anxiety
- disfigurement
- difficulties with eating
- difficulties with speaking
- changes in sexual activity
You may have got through the diagnosis and treatment for nasopharyngeal cancer, but you may be finding it difficult to deal with some of the side effects of treatment. Speak with you doctor about any difficulties you may be experiencing. Your doctor may give you a referral to a psychologist or another healthcare professional who can help you. Speak with your family and friends too about any concerns you may have.
You may find it helps to join a patient support group and speak with others who are having treatment for head and neck cancer. See our Find Support database.
You can also find help and advice in online self-help resources such as beyondblue.
For more information about coping with cancer visit Cancer Council Australia.
On this page