Your doctor will look inside your nose and throat using a very thin flexible tube with a tiny light and camera on it (called an endoscope). This can be done in an office or clinic.
Nasopharyngeal Cancer
Introduction
What is Nasopharyngeal Cancer?
Nasopharyngeal Cancer is a type of Throat Cancer that starts in or behind the nose. If it's not the cancer type you're looking for, please explore the information about other types of Throat Cancers or other types of Head and Neck Cancers.
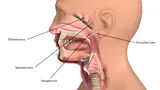
Nasopharyngeal Cancer is a type of Throat Cancer that forms in the nasopharynx, which is highest part of the throat — in or behind the nose.
Cancer occurs when cells become abnormal, grow uncontrollably and have the potential to spread to other parts of the body. These cells build up to form a mass (or lump).
Watch this 3D video explainer about Nasopharyngeal Cancer:
What is the nasopharynx?
The pharynx is the medical term for the throat. It has three parts:
- nasopharynx (upper throat)
- oropharynx (mid throat, including the tonsils)
- hypopharynx (lower throat).
The nasopharynx is the highest part of the throat. It is the airway behind the nose and above the top of the mouth (soft palate).
What does the nasopharynx do?
The nasopharynx connects the nose (nasal) cavity to the space behind the mouth (the oropharynx).
The nasopharynx allows air breathed into the nose to go down through the voice box (larynx) and into the lungs. It also allows phlegm (mucus) from the nose to be swallowed or spat out.
What causes Nasopharyngeal Cancer?
Doctors often can’t explain why a person gets cancer. But we do know what makes some cancers more likely.
The main causes of Nasopharyngeal Cancer are:
- Viruses — in particular the Epstein-Barr virus (EBV)
- Smoking (cigarettes, cigars or pipes) or using smokeless tobacco (snuff and chewing tobacco) — If a person smokes or has smoked in the past they have a higher risk of getting nasopharyngeal cancer than someone who has never smoke. Get information about quitting smoking.
Other factors that increase the risk of Nasopharyngeal Cancer are:
- Age — Most nasopharyngeal cancers are in people aged 40 years and over
- Being male — In Australia, men are about three times more likely than women to get nasopharyngeal cancer
- Being from Southern China or South East Asia — People from Southern China and South East Asia seem to have a higher risk
- Eating a lot of salt, cured fish and meat
Symptoms and Signs of Nasopharyngeal Cancer
The signs and symptoms of Nasopharyngeal Cancer depend on where the cancer is, its size and how far it has spread in the body.
Common signs and symptoms include:
- nasal obstruction or stuffiness
- frequent nose bleeds
- blocked ear, decreased hearing or ringing in the ear (especially on one side only)
- a lump in the neck
- frequent headaches
- numbness in the face
- blurred or double vision
Most often these symptoms are not from Nasopharyngeal Cancer. However, if you have any of these symptoms for more than a few weeks, talk to your doctor as early as possible. They may be able to help diagnose and treat you.
What are the tests for Nasopharyngeal Cancer?
It is important that your doctor establishes the diagnosis of Nasopharyngeal Cancer, assesses the size of the cancer and whether it has spread to the lymph nodes in the neck or elsewhere in the body.
To answer these questions your doctor will need to do the following things:
- ask about your medical history including signs you may have noticed, any other health conditions, medications that you are taking, and whether you smoke or drink alcohol
- perform a physical examination by feeling and looking inside your throat and neck
- order diagnostic tests, which may include scans. .
Not everyone will need to have every test for Nasopharyngeal Cancer. Your doctor will recommend the tests that are right for you. The most common tests for Nasopharyngeal Cancer are:
This involves taking a piece of tissue (sample) either from the throat or from a lymph node in the neck, if it appears to be involved by the cancer. A pathologist then looks at the sample under a microscope to check for cancer cells. This is often the only sure way to tell if you have cancer. If the suspicious area can be safely accessed through the mouth, your doctor may take a sample for biopsy in the office. However, this is often not possible because the cancer may be too far back and some patients need to be asleep under a general anaesthetic for the biopsy. This is usually done as a day procedure.
Your doctor may order one of two types of biopsies of the lymph nodes in your neck. Both are usually done using an ultrasound scan to make sure the needle is in the right spot.
Fine Needle Aspiration or FNA is used when there is a lump (enlarged lymph node) in the neck that could have cancer cells in it. During the procedure, your doctor will take some cells from the lump using a needle. It may feel a bit uncomfortable during the biopsy.
Core biopsy uses a bigger needle to get more cells for the biopsy. This is more uncomfortable than needle biopsy so doctors only use this if it is really needed.
This uses X-rays to take pictures of the inside of the body. If a person has cancer, a CT scan can help the doctor to see where it is, measure how big it is, and if it has spread into nearby organs or other parts of the body.
MRI (Magnetic Resonance Imaging) Scan
This uses magnetic fields to take pictures of the inside of the body. This helps your doctor see how far a cancer has grown into the tissue around it.
PET (Positron Emission Tomography) Scan
This is a whole body scan that uses a radioactive form of sugar which can show if nasopharyngeal cancer has spread to the lymph nodes or elsewhere in the body.
Treatment Options for Nasopharyngeal Cancer
Following a diagnosis of Nasopharyngeal Cancer, your cancer care team will discuss the treatment options, including the possibility of participating in a clinical trial, that are suitable for you. This is also a good time to consider if you would like a second opinion.
The most suitable treatment for Nasopharygneal Cancer depends on many things including:
- size and location of the cancer
- whether the cancer has spread
- personal factors (e.g. age, general health and treatment history)
- treatments available (and whether any clinical trials are available)
- your preferences for treatment
There are three types of treatment available for Nasopharyngeal Cancer. These include:
- Radiation therapy
- Chemotherapy
- Surgery
Radiation Therapy for Nasopharyngeal Cancer
Radiation Therapy is the main treatment for Nasopharyngeal Cancer.
It uses high-energy waves to destroy or damage cancer cells. The most common radiation therapy approach for Nasopharyngeal Cancer is called external beam radiation. This type of radiation therapy applies radiation from outside the body.
Radiation Therapy may be given using:
- Intensity Modulated radiation Therapy (IMRT) or Volumetric Arc Therapy (VMAT) or Tomotherapy, which use different ways to deliver radiation very precisely, minimising the radiation that gets to healthy parts of the body surrounding the cancer.
- Stereotactic Radiation Therapy which delivers a large and precise dose of radiation in one or a few visits. It can be used as part of radiation therapy to increase the dose of radiation to the nasopharynx cancer. It is sometimes used to treat cancer that has come back.
Radiation Therapy for Nasopharyngeal Cancer can be used definitively or palliatively.
- Definitive Radiation Therapy: is the main treatment for nasopharyngeal cancer. It is used without surgery to cure nasopharyngeal cancer. Typically, radiation therapy is delivered daily (but not on weekends) over 7 weeks. Sometimes chemotherapy is added to radiation therapy (chemoradiation) to make it more effective.
- Palliative Radiation Therapy: in cases where a cure is not possible, radiation therapy is used to relieve symptoms of advanced nasopharyngeal cancer. Symptoms that may require palliative radiation therapy include pain, bleeding and pressure symptoms from the cancer pressing on vital structures (e.g. visual disturbance and headaches).
How do I prepare for Radiation Therapy?
You will meet with many members of the cancer care team, who will help you learn how to look after yourself through radiation therapy, recovery and long term follow-up. They will also talk to you about side effects and how to manage them. It may be helpful to write down questions as they come up, so you can ask anyone in your cancer care team when you see them.
Radiation Therapy Mask-Making and Simulation
- Radiation therapy is a precise treatment. In order to make sure, that the cancer is covered by the treatment, you will need to be very still during the treatment, usually for about five minutes. A radiation therapy mask that is made to fit perfectly to your shape, will be put on you during each treatment to help the machine target where the cancer is.
- You will have a planning CT scan (and sometimes other scans) with the mask on. Your radiation oncologist and radiation therapists will use these scans with all your other clinical information to develop a radiation therapy plan just for you (a personalised plan). Your plan will be checked by the radiation therapy and radiation oncology physics team before it is ready to be used for your treatment. This whole process can take approximately 2-3 weeks.
You might need to have some of your teeth taken out, this will depend on the area being treated and the dose of radiation therapy. It is important to take out any broken or infected teeth before radiation therapy. Taking out unhealthy teeth after radiation therapy can cause problems with the jaw bone.
Diet, Nutrition and the role of your Dietitian
Your cancer and its treatment can make it hard to eat and drink. Your doctor will recommend you see a dietitian to maximise your nutrition during treatment as well as while you are recovering. Sometime feeding tubes may be recommended depending on the area being treated and the dose of radiation therapy. There are two common types of feeding tubes:
-
Gastrostomy tube (sometimes called a PEG tube): this type of tube is inserted through your abdominal wall into your stomach, with part of the tube staying outside the stomach. A syringe can be attached to the tube to give you food this way if needed. The tube is inserted using a camera through the mouth into the stomach (gastroscopy) or using a CT scanner to guide insertion directly through the skin. If a PEG tube is needed, your doctor will organise this before starting your radiation therapy
-
Nasogastric tube: this type of tube goes through the nose down into the stomach and is usually used for short periods (days or weeks). A nasogastric tube can be inserted at any time (before, during or after treatment).
Your cancer and its treatment can make swallowing and speech difficult. Your doctor will recommend you see a speech pathologist, who can help you with ways to manage swallowing and communication difficulties, during and after treatment.
There are many other aspects of supportive care that are available, ask your doctor if you have any specific needs.
Side Effects
The side-effects of radiation therapy start around two weeks into treatment and progress through treatment to peak in the last week or just after treatment ends. The side effects start to improve 2-3 weeks after the end of treatment.
Side effects associated with radiation therapy depend on:
- the dose of radiation therapy
- the area being treated
- whether or not chemotherapy is added to the radiation
Each person responds to radiation therapy differently. Some people may experience a few side effects while others may not experience any at all. The following are some common side effects of radiation therapy.
- tiredness
- skin irritation in the treated area e.g. redness, dryness and itching, weeping skin, scaling or sometimes skin breakdown (sores)
- nasal irritation, blockage and crusting
- ulcers in the mouth and throat that make it painful or difficult to chew or swallow
- sticky or thick saliva
- altered taste, which is usually a loss of taste or, sometimes, an unpleasant taste in the mouth
- blocked ears from inflammation within ear canals
Most side effects are short lived and may go away within 4–6 weeks of finishing radiation therapy. Some side effects may last for months after you finish radiation therapy and some may be permanent.
Long-term side effects of radiation therapy include:
- dry mouth (called xerostomia) and difficulty eating dry food such as bread/biscuits due to lack of saliva. With modern radiation techniques, some recovery of saliva may be expected up to two years after radiation therapy
- inability to eat certain foods, in particular sensitivity to spicy or acidic foods
- gum and tooth problems from lack of saliva
- crusty nasal discharge
- worse hearing or deafness may occur, although with modern radiation therapy techniques the risk of this side effect can be greatly reduced
- underactive thyroid gland
Rare side effects from nerve damage (called cranial neuropathy) may occur following treatment of very advanced cancers. These include difficulty speaking, swallowing, impaired and double vision. This is because the nasopharynx is very close to a number of important parts of the nervous system (e.g. spinal cord, brain and nerves) involved with seeing, hearing and balance.
The risk of these rare side effects is very low and with modern radiation therapy techniques, your radiation oncologist will be very careful to avoid these structures by using very precise radiation therapy techniques. You can talk to your radiation oncologist to find out if these concerns apply to your situation and to find out more about these rare side effects.
Once your radiation therapy ends, you may continue to have follow-up appointments so that your doctor can check your recovery and monitor any side effects that you may have. Usually your doctor may arrange for a PET scan about 12 weeks after finishing radiation therapy to make sure the cancer has completely gone.
Your doctor may recommend that you receive specific supportive care to help during your treatment and recovery.
Chemotherapy for Nasopharyngeal Cancer
Chemotherapy uses medicines to destroy or damage cancer cells. For Nasopharyngeal Cancers, chemotherapy is usually given into a vein through a needle with a cannula (tube) attached.
Chemotherapy is usually given during radiation therapy for advanced stage cancers to help the radiation therapy work better. This is called concurrent chemoradiation.
There are a number of different types of chemotherapy that may be used to treat Nasopharyngeal Cancers:
Neo-adjuvant
This is when chemotherapy is given before radiation therapy to help shrink large cancers and make them easier to target with radiation therapy. Sometimes chemotherapy is added to definitive radiation therapy (chemoradiation).
Adjuvant
This is when chemotherapy is given after surgery, usually in combination with radiation therapy (called concurrent chemoradiation). It is usually given once a week during radiation treatment. Adding chemotherapy makes the radiation more effective at destroying cancer cells, but also leads to increased side effects for most patients.
Definitive
Sometimes chemotherapy is added to definitive radiation therapy (chemoradiation). It is usually used for advanced stage nasopharyngeal cancers. This may be given once every 3 weeks or once a week throughout the duration of radiation therapy. This makes the radiation more effective at killing cancer cells but also leads to more side effects in most people.
Palliative
In cases where cancer is considered incurable, because it may be too large or has spread too much to be removed by surgery, palliative chemotherapy may be suitable. Palliative chemotherapy does not aim to cure a cancer, but helps to slow the growth of cancer and reduce symptoms. It is important to remember that palliative chemotherapy is not as intense as other types and is much less likely to have significant side effects.
Before you start treatment, your medical oncologist will choose one or more chemotherapy medication that will be best to treat the type of cancer you have. The particular chemotherapy medications used will depend on:
- whether the treatment is curative or palliative
- when it is used
- your medical history
Side Effects
The side effects of chemotherapy depend on the medication used and and how much you are given by your doctor (the dose). The most common medications are cisplatin, carboplatin and 5-Fluoruracil (5-FU).
Each person responds to chemotherapy differently. Some people may experience a few side effects while others may not experience any at all. The following are common side effects of chemotherapy:
- a feeling of wanting to vomit (nausea) or vomiting
- more side effects of radiation, if you have chemotherapy at the same time as radiation
- loss of feeling in the fingers and toes
- kidney damage (caused by some medications)
- hearing loss/thinning
- ringing in the ears
- rash
- higher risk of infection (if the chemotherapy reduces the number of white cells in the blood).
Most side effects are short lived and may go away once you finish chemotherapy. Some side effects can take months to years to improve or may be permanent.
Once your treatment ends, you will have regular follow-up appointments so that your doctor can check your recovery, make sure the cancer has not returned and monitor and treat any side effects that you may have. Your doctor may recommend that you receive supportive care to help during your recovery.
Surgery for Nasopharyngeal Cancer
Surgery for Nasopharyngeal Cancer is not common because the area is difficult to get to and it is close to important nerves and blood vessels.
Surgery may be needed, if the cancer returns after previous treatment with radiation therapy.
How can I prepare for the surgery?
Your doctor will explain details of the surgery, general risks and side effects of surgery. Ask your doctor if you have questions. They may recommend:
- stopping blood thinners (e.g. aspirin) before surgery to reduce the risk of bleeding
- special stockings to reduce the risk of blood clots
- early mobilisation (i.e. not staying in bed) to reduce the risk of blood clots and chest infection
- antibiotics to lower the risk of wound infection.
If you smoke, it is important that you consider stopping smoking before starting treatment to help reduce the risk of infection and help you recover after your treatment.
Surgical Procedures
The type of surgery used in this situation will depend on the size and location of the recurrent cancer.
Download PDF - Endoscopic Sinus Surgery
This is where a telescope and surgical instruments are passed through the nose to get to the nasopharynx without external cuts.
Download PDF - Maxillary Swing
This is where a cut is made in the upper lip and next to the nose, and the upper jaw is cut to allow the surgeon to get access to the nasopharynx.
Download PDF - Neck Dissection
Download PDF - Return to Activity Following Neck Dissection
This involves removal of lymph nodes from the neck. It is used to take out lymph nodes that have not responded to radiation therapy or to treat cancer that has come back after earlier treatment.
Side Effects of Surgery
Treatment for Nasopharyngeal Cancer may lead to a number of side effects. You may not experience all of the side effects. Speak with your doctor if you have any questions or concerns about treatment side effects.
Questions to Ask
- Exactly what type of Nasopharyngeal cancer do I have? Where is it located?
- Why did I get this cancer? Is it related to the HPV virus?
- What stage is the cancer?
- What are my treatment options? Which treatment do you recommend for me and why?
- Have you discussed my case at a Multidisciplinary Team meeting and what were the recommendations?
- Who will be part of the cancer care team, and what does each person do?
- Should I see another specialist before treatment, such as a radiation oncologist, medical oncologist, plastic surgeon, dentist, dietician or speech pathologist?
- What are the possible side effects of treatment in the short- and long-term? How can they be prevented or managed?
- Will the treatment affect my ability to eat, swallow, or speak? Will I need a feeding tube?
- What will happen if I don't have any treatment?
- How much will the treatment and/or operation cost? Will Medicare or my health insurance cover it?
- What follow-up tests will I need? How often will they be?
- Am I suitable for any clinical trials?
- What lifestyle changes (diet, exercise) do you recommend I make
- Who can I call if I have any problems or questions?
- Where can I find emotional support for me and my family? Is there a support group or psychologist you can recommend?
- If I wanted to get a second opinion, can you provide all my medical details? Do you mind if I get a second opinion?
Follow-Up Care
You will need regular check-up of your nose, throat and neck after treatment for Nasopharyngeal Cancer. This will include a physical exam and checking your nose and throat using a thin, flexible tube with a light and camera (nasendoscopy). Some people may also need imaging of their nose and throat using CT, MRI or PET scans during follow-up. It is important to keep up with follow-up appointments to make sure that if the cancer comes back it is caught early and can be treated. If you have any concerns between appointments you should contact your doctor.
People who smoke and/or drink alcohol can reduce the risk of their cancer coming back or getting a new cancer if they quit smoking and reduce the amount of alcohol they drink. Ask your cancer care team for advice if this applies to you.
Importance of Ongoing Dental Care
A dentist plays an important role in your head and neck cancer treatment. Side-effects can often be prevented or reduced through regular dental check-ups before, during and after cancer treatment.
After your treatment, you should visit the dentist every six months for a check-up because the side effects of radiation therapy on your teeth can last for your whole life.
Mental Health for People with Cancer
Sometimes this is referred to as psychosocial aspects or survivorship.
Being diagnosed with cancer and having treatment can lead to extra worries or concerns for you and the people caring for you. Depending on the treatment, you may experience any of the following:
- low mood or depression
- anxiety
- disfigurement
- difficulties with eating
- difficulties with speaking
- changes in sexual activity
You may have got through the diagnosis and treatment for mouth cancer, but you may be finding it difficult to deal with some of the side effects of treatment. Speak with you doctor about any difficulties you may be experiencing. Your doctor may give you a referral to a psychologist or another healthcare professional who can help you.
For more information about coping with cancer visit Cancer Council Australia.
On this page